We walked in today as Alida was getting her chest tubes removed. Her drainage was down to 20ml so they felt comfortable removing them. They plan to remove her subclavian central line and put a PICC line in one of her lower extremities tomorrow. When they do the line change they will also pull her external pacing leads (blue wires on her belly in the photos below). They ended the fentanyl last night. If everything goes well after switching to the PICC line tomorrow, they may extubate her in the afternoon. Her vent settings are down to a rate of 10 and oxygen percentage of 35% (room air is 21%). She is still having a few irregular heart rhythms that they are going to watch and determine if her pacemaker needs anymore adjustments. It’s nice seeing her with a few less tubes and her chest incision looks great.

We got to see her chest X-ray this morning. It was our first time seeing the pacemaker size in relation to her body as well as it’s positioning. This is NOT Alida, but it gives you a general idea of what the chest X-Ray looked like. We could also see the wires holding her sternum together, which this patient doesn’t have.
It’s snowing today which makes it feel a little more like Christmas time. We are able to enjoy it since we are only getting a few inches down here, instead of several feet. This is the view from Alida’s hospital room.
We are enjoying our stay at the Ronald house. It is under construction. They are doubling the size of it plus renovating existing portions. They just finished the communal kitchen on the floor above us. It is beautiful.
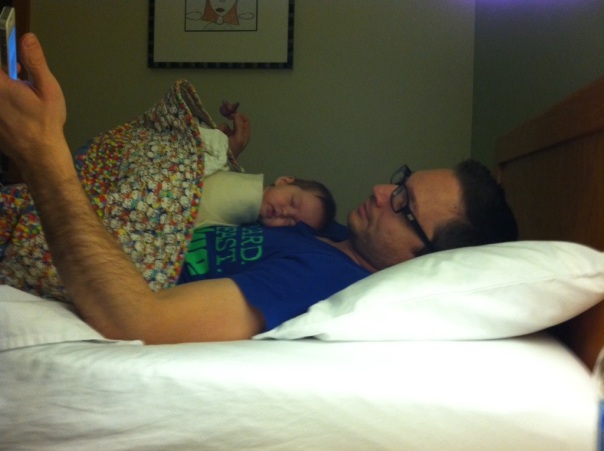
The room is small with two single beds and the hardest memory foam we have ever slept on. Brian jumped onto bed on his side last night with quite the thud. We were joking that if you jumped too high and hard into bed, you might break your clavicle or throw out your shoulder or back. We will keep this in mind over the next few weeks during our bed jumping escapades. Brian did settle in with Lucie last night after the memory foam relaxed a little.
Brian is growing some facial hair for the first time in his life. I told him her needs to wait until at least Wednesday to shave.

We continue to take it one day at a time, celebrate the small victories, and enjoy each other’s company. Happy Sunday!